Decompression Illness in Sports Divers: Part I
Ernest S. Campbell, MD, FACS, Orange Beach, Ala.
Medscape Orthopaedics & Sports Medicine eJournal 1(5), 1997. © 1997 Medscape Portals, Inc
Abstract and Introduction
Abstract
Decompression sickness (DCS) results from gas coming out of solution in the bodily fluids and tissues when a diver ascends too quickly. This occurs because decreasing pressure lowers the solubility of gas in liquid. Also, the expansion of gas in the lungs may lead to alveolar rupture, also known as "Pulmonary Overinflation Syndrome," which may, in turn, result in arterial gas embolism (AGE). DCS, AGE, and all of their presentations are grouped together under the heading "decompression illness." Joint pain is the most common complaint in DCS, especially in the elbow, shoulder, hip and knee. Blockage of vessels results in ischemia and infarction of tissues beyond the obstruction, and inflammatory changes can lead to extravasation into the tissues, resulting in edema and further compromising the circulation. Involved skin displays a mottled appearance known as "cutis marmorata." In the lymphatic system, bubbles may result in regional lymphedema. More severe cases may involve the brain, the spinal cord, or the cardiopulmonary system. Neurologic manifestations may include sensory deficits, hemiplegia, paraplegia, paresthesias, and peripheral neuropathies. Possible cardiopulmonary effects include massive pulmonary gas emboli or myocardial infarction. Decompression sickness is treated with recompression in a chamber to 60 FSW or deeper, associated with hyperbaric oxygen breathing. In the US, this therapy is usually guided by a Navy Treatment Table. These tables are very effective, especially when recompression is begun promptly.
Introduction
On the earth's surface, the human body is exposed to an ambient pressure which is the result of the combined partial pressures of all the gases in the earth's atmosphere. At sea level, the force of this pressure is described as 1 atmosphere absolute (ATA). As a diver descends, exposure to increasing pressure forces more gas to dissolve in the bodily fluids and tissues, as described by natural gas laws. Upon ascent through the water column, the solubility decreases again. Rapid ascent may lead to bubble formation and decompression sickness (DCS) or alveolar rupture ("Pulmonary Overinflation Syndrome" [POIS]), with resultant bubbles in the arterial circulation (arterial gas embolism [AGE]).[1]DCS, AGE, and all of their presentations are grouped together under the heading "decompression illness" (DCI).[2] Treatment consists of recompression in a chamber using air and 100% oxygen. Bubbles may form in blood vessels, where they may cause ischemia and infarct, and in tissues, where they may initiate an inflammatory response. Inflammatory changes can lead to extravasation into the tissues, further compromising the circulation and resulting in edema.
Hyperbaric exposures (situations where there are elevated pressures) can occur during construction and tunneling projects, in hyperbaric oxygen treatment facilities and in aviation. (The airman is subject to the same problem as divers, except that the situation is reversed--bubbles form on ascent, due to a decrease in pressure and supersaturation. Returning to the ground increases pressure and is analogous to recompression. However, DCS symptoms may occur after returning to the ground and sometimes require additional recompression.)
Recreational scuba diving is the most common type of hyperbaric exposure, especially since the explosive growth of sports scuba (self-contained underwater breathing apparatus) diving in the past decade. Hyperbaric oxygen (HBO) treatment is gaining popularity as the definitive therapy for a growing number of disorders, including decompression sickness, AGE, CO poisoning, clostridial infections, crush injuries, diabetic leg ulcers, skin graft failures, refractory osteomyelitis, thermal burns, necrotizing soft tissue infections, and osteoradionecrosis.
It is incumbent on physicians to be fully conversant with the diagnosis and treatment of decompression illness, especially because the hyperbaric chamber is now widely recognized as effective in reversing the sometimes-deadly changes that take place with DCI.
Hyperbaric Terminology and Physics
At sea level, the body is exposed to 1 ATA of pressure. This is also expressed as 760 millimeters of mercury (mm Hg), 33 feet of sea water (FSW), or 14.7 pounds per square inch (psi). The normal atmospheric pressure of 1 ATA is actually a reference point. When one states that systolic blood pressure is 120 mm Hg, we are really saying that it is 120 mm Hg above that of the surrounding environment which is 880 mm Hg (absolute pressure). The systolic blood pressure is a "gauge" pressure, meaning that the pressure displayed is the actual pressure minus the constant 1 ATA of atmospheric pressure. By analogy, the depth gauge of a diver reads "0" on the surface but he is exposed to 1 ATA or the same as 33 FSW--at 33 feet underwater he will be under 2 atmospheres of absolute pressure.A fluid-filled space or a solid organ will not change in size as pressure changes because fluids are not compressible. A space with elastic walls that is filled with air will change shape according to Boyle's law,[3] which states that the volume of gas is inversely proportional to the absolute pressure (Fig. 1). For example, a balloon filled with one cubic foot of air on the surface (1 ATA) would shrink to a volume of one-half cubic foot if taken to a depth of 33 FSW (2 ATA), and to one-fourth of a cubic foot at 99 FSW (4 ATA).

Figure 1. Boyle's law states that the volume of gas is inversely proportional to the absolute pressure when temperature is constant. Therefore, divers are taught to exhale on ascent--otherwise expanding air may rupture the delicate alveoli. Adapted from NOAA (1979).
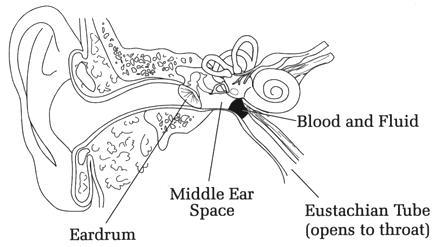
The gas-filled organs--such as the middle ear or the lungs--have only a limited capacity to change their volume. As long as the quantity of gas within the space is vented to compensate for changes in pressure, there are no problems. Thus, divers are taught to exhale on ascent--otherwise the expanding air may rupture the delicate alveoli--and to clear their ears on descent, which adds gas to the middle ears to prevent collapse. If this equalization is not performed, "barotrauma" occurs--an "ear squeeze" (Fig. 2) in the case of the ear, and ruptured alveoli or POIS and possibly AGE in the case of the lung.
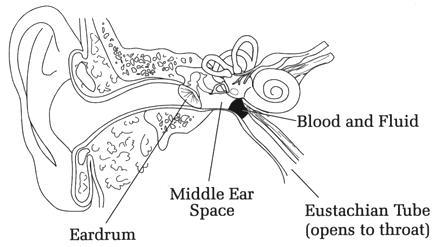
Figure 2. Divers are taught to clear their ears on descent, which adds gas to the middle ears to prevent collapse. If this equalization is not performed an "ear squeeze" may occur. Note that the eardrum is retracted and the Eustachian tube is blocked by blood and fluid. Reprinted with permission from Scuba Diving Explained: Questions and Answers on Physiology and Medical Aspects of Scuba Diving, Lawrence Martin, MD.
Henry's law and Dalton's law are central to understanding decompression sickness. Henry's law states that, at a given temperature, the amount of gas that will dissolve in a liquid is directly proportional to the partial pressure of the gas. Dalton's Law states that the pressure of a gas is the sum of the partial pressures of all gases present.Nitrogen , which comprises 78% of atmospheric gas and is biologically inert, is the gas which leads to pathology as it follows the gas laws in the vessels and organs of a scuba diving human. As a diver breathing air from a tank descends, the increased pressure causes more nitrogen to enter his tissues than was present at the surface. If enough nitrogen enters into solution and the diver returns to the surface too quickly, the excess gas will not have a chance to be eliminated ("blown off") gradually through the lungs. The nitrogen will then come out of solution and go into a gas phase--bubbles, which form in the blood and tissues of the body. These bubbles account for the clinical entity that we call decompression sickness (DCS).
Decompression Sickness
Pathophysiology. The amount of nitrogen that diffuses into the bodily tissues during a dive depends on the depth of the dive and the duration of exposure. On ascent, as the body experiences a rapid reduction in ambient pressure, biologically inert gases that are dissolved in the tissues may come out of solution as bubbles if the diver does not allow adequate time for the excess nitrogen to be eliminated through respiration. (For repetitive dives, the diver must consider the nitrogen retained from previous dives in order to select a safe decompression schedule.) Visualize the bubbling froth of CO2 that rushes out of solution from the sudden decrease in pressure that occurs when you open a can of soda pop. The bubbles in the body may form in the venous blood, musculoskeletal system or other body tissues; decompression sickness is the clinical condition that results.Systemic manifestations. Decompression sickness, as would be expected, is a multisystem disease. Joint pain is the most common complaint in DCS, with pain in the elbow, shoulder, hip and knee joints being the most prevalent sites.[4,5,6] The skin may be involved, displaying a mottled appearance known as "cutis marmorata" (Fig. 3). Bubbles in the lymphatic system may result in regional lymphedema. Cases of decompression sickness limited to musculoskeletal, skin, or lymphatic manifestations are often referred to as Type I DCS.

Figure 3. Cutis marmorata is a mottled appearance of the skin seen in type I decompression sickness.
More severe cases may involve the brain, the spinal cord, or the cardiopulmonary system.[7] Neurologic manifestations may include sensory deficits, hemiplegia, paraplegia, paresthesias, and peripheral neuropathies.[8] Possible cardiopulmonary effects include massive pulmonary gas emboli or myocardial infarction. Decompression sickness with neurologic or cardiopulmonary symptoms is often referred to as Type II DCS.The presenting symptoms of DCS are influenced by the depth of the dive and the bottom time of the dive, the inert gas breathed, the adequacy of decompression, and the delay to presentation.
The US Navy Diving Manual notes that the majority of DCS cases involve musculoskeletal pain.[8] Thalmann and colleagues[9-12] reported that even relatively risky experimental dive series conducted by the navy to develop new decompression tables and decompression computer programs had a predominance of Type I symptoms (106 cases of Type I as compared to 37 cases of Type II DCS).
In contrast to this, recreational reports have a higher incidence of more serious symptoms. Kizer[13] published a series of 50 cases and noted 24 patients with Type I and 26 with Type II DCS. Diving fishermen in Singapore with a significant delay in recompression had a much higher incidence of serious cases than previous reports, with 47 out of 58 patients experiencing Type II DCS.[14]
Prevention. Important questions for divers include "how quickly should I rise?" and "how long should I stay on the surface between dives?" The various dive tables developed by governmental and diving instruction agencies attempt to answer these questions. The US Navy Decompression Tables were compiled after studying the effect of decompression on young, fit men and have been found in some cases not to apply to the average recreational diver. These tables are being revised; the training agencies PADI (Professional Association of Diving Instructors), in Canada, the DCIEM (Defense and Civil Institute of Environmental Medicine) (Table I), and the NAUI (National Association of Underwater Instructors) (Table II, III, IV, and V), all have different diving tables which attempt to meet this need for more conservative decompression schedules. This is accomplished in part by shortening the allowable bottom time for no-decompression diving (No-D diving).
Adherence to appropriate decompression tables and dive computers reduces the risk of DCS, but does not eliminate it entirely. Many cases of DCS have been reported in divers who have been decompressed in strict compliance with published tables. In the navy, the incidence of DCS is variously reported between 0.01% and 1.25%.[3]
Both dive computers and tables are tools that can help the diver understand the dive profiles they are conducting. Adherence to dive schedules does not guarantee DCS will not occur. "It doesn't matter which dive tables you don't use" is an apt phrase coined by Neuman. Shallow divers are at less risk, but they can still become saturated with nitrogen if they use more than one tank of compressed air, and will still need to off-gas as they ascend in the water column.
Treatment. Decompression sickness is treated with recompression in a chamber to 60 FSW or deeper associated with hyperbaric oxygen breathing.[15] In the US, this therapy is usually guided by a Navy Treatment Table.[8] These tables are very effective, especially when recompression is begun promptly.[16]
The purpose of the therapy called for in the Navy Treatment Tables is two-fold: to promote inert gas elimination and to help cause a decrease in bubble size. The treatment outlined by the tables also provides oxygen to the damaged tissues, treats platelet and clotting damage and allows excretion of harmful metabolites. The oxygen reduces CNS edema and provides a high oxygen gradient (2000 mm Hg) for the ischemic tissues.[17]
Specifics: Recompression treatment of decompression sickness. First, it is important to take the time for a careful clinical exam, because true Type I DCS without other manifestations is very rare, and diagnostic tests are of little value.
The initial therapy for Type I and Type II DCS is treatment in a chamber with Navy Treatment Table 6 ( Table VI ). Table 6 indicates recompression to 60 feet for 285 minutes, with intermittent oxygen breathing periods and slow "ascent to the surface." (The diving tables indicate increases in pressure with the word "descent" and decreases with "ascent." They also give their pressure values in depth-equivalents.) The periods of oxygen breathing are broken up into intervals to prevent O2 toxicity ( Table VI ). If O2 seizures occur, turn off the O2for 15 minutes and continue the treatment.
In the case of poor response to standard Navy Treatment Tables 6A ( Table VII ) or 6 ( Table VI ), Treatment Table 6 ( Table VI ) can be extended for additional oxygen breathing periods at 60 or 30 feet. If you are following Treatment Table 6A ( Table VII ) and there is no resolution or the patient is getting worse on ascent, try Treatment Table 4 ( Table VIII ) , which indicates staying at 165 feet for 2 hours--then go to Table 6 at 60 feet with extensions, if necessary.
Treatment Table 7 ( Table IX ) is used for worsening or unresolved DCS or AGE. It is a long, involved and dangerous treatment and should not be used unless adequate support is available. If all else fails, call Divers Alert Network (DAN) at (919) 684-9111, rather than creating your own treatment table.
Even after "successful" treatment, some people experience relapse of symptoms. Recurrences are treated with Treatment Table 5 ( Table X ) or Treatment Table 6 ( Table VI ) once or twice-daily until no further improvement is observed by the medical director of the facility. Recent evidence indicates that persistent neurologic defects may be lessened by repetitive treatments on Navy Treatment Tables 5, 6 (Tables X , VI ) or even with 100% oxygen at 30 FSW for 90 minutes bid. Flying should be avoided for a period of 72 hours after treatment for DCS or AGE.
Equipment which might be needed in the altered pressure environment includes ventilators, bubble traps and pumps for use with intravenous catheters, endotracheal tube cuffs which inflate with water, and if chest tubes are required, the patient must be vented during descent using #18 gauge 1 1/2 " needle.
Arterial Gas Embolism
Pathophysiology. Arterial gas embolism (AGE) is another disorder in which bubble formation may occur in the vascular system.[18] The bubbles in AGE originate not from supersaturation of gases in the blood and tissues but from rupture of the alveoli due to the barotrauma of ascent. The bubbles enter the pulmonary venous system and are carried to the heart and arterial systemic circulation.Systemic symptoms. As might be expected, most symptoms from this disorder are localized to the cerebral circulation (Fig. 4), with occasional embolization to the coronary arteries causing cardiac arrest. Classically, the presentation is that of sudden onset of unconsciousness within minutes of reaching the surface after a dive--there having been some reason why the diver ascended with his glottis closed (unconsciousness, panic, dry suit blowup, loss of weights, malfunction of buoyancy compensator). Other possible presentations include hemispheric motor and/or sensory deficits, confusion and convulsion. Peripheral nerve changes and musculoskeletal pain are not part of the symptom complex of AGE.[19-21]

Figure 4. Most symptoms from arterial gas embolism are due to the effect of air bubbles in the cerebral circulation, with occasional embolization to the coronary arteries, causing cardiac arrest. Pathway for the development of cerebral gas embolism is shown. Reprinted from the NOAA.
Treatment. Management is generally similar to that of DCS--recompression and HBO are indicated in all cases as quickly as possible.[22]Specifics: Recompression treatment of gas embolism. In contrast to the treatment of decompression sickness, one should not delay for diagnostic work-up or extensive clinical evaluation. Instead, the first question is whether to use Treatment Table 6A or 6 (Tables VII , VI ). If there is a delay greater than 4 hours, Treatment Table 6 ( Table VI ) should be used initially and then proceed to 6A ( Table VII ) depending on the clinical response. Treatment Table 6A ( Table VII ) allows for rapid compression to 165 feet and is used for major air embolisms. If such a chamber is not available, then one should use a 3 ATA chamber.
For those patients not responding to Navy Table 6 ( Table VI ), other choices are available: US Navy Table Treatment 4 ( Table VIII ) or the Comex Table, which prescribes 30 minutes breathing 50/50 O2/N2 mix at 100 feet. Unproven treatment schedules should be avoided, but extensions to the tables are not experimental and should be used as necessary.
Tables
Table I. Short Form of the DCIEM Tables (front)
Table II. NAUI Dive Tables
Table III. NAUI Dive Table 1
Table IV. NAUI Dive Table 2
Table V. NAUI Dive Table 3
Table VI. US Navy Treatment Table 6: Oxygen Treatment of Type II Decompression Sickness*¶
Depth
(feet) | Time
(minutes) | Breathing
Media¥ | Total
Elapsed
Time (hr:min) |
|---|
| 60† | 20 | O2§ | 0:20‡ |
| 60 | 5 | Air | 0:25 |
| 60 | 20 | O2 | 0:45 |
| 60 | 5 | Air | 0:50 |
| 60 | 20 | O2 | 1:10 |
| 60 | 5 | Air | 1:15 |
| 60 to 30 | 30 | O2 | 1:45 |
| 30 | 15 | Air | 2:00 |
| 30 | 60 | O2 | 3:00 |
| 30 | 15 | Air | 3:15 |
| 30 | 60 | O2 | 4:15 |
| 30 to 0 | 30 | O2 | 4:45 |
| * | Treatment of Type II or Type I decompression sickness when symptoms are not relieved within 10 minutes at 60 feet. |
| † | Descent rate--25 ft/min. Ascent rate--1 ft/min. Do not compensate for slower ascent rates. Compensate for faster rates by halting the ascent. |
| ‡ | Time at 60 feet begins on arrival at 60 feet. |
| § | If oxygen must be interrupted because of adverse reaction, allow 15 minutes after the reaction has entirely subsided and resume schedule at point of interruption. |
| ¥ | Caregiver breathes air throughout unless he has had a hyperbaric exposure within the past 12 hours, in which case he breathes oxygen at 30 feet. |
| ¶ | Extensions to Table 6: Table 6 can be lengthened up to 2 additional 25 minute oxygen breathing periods at 60 feet (20 minutes on oxygen and 5 minutes on air) or up to 2 additional 75 minute oxygen breathing periods at 30 feet (15 minutes on air and 60 minutes on oxygen) or both. If Table 6 is extended only once at either 60 or 30 feet, the tender breathes oxygen during the ascent from 30 feet to the surface. If more than one extension is done, the caregiver begins oxygen breathing for the last hour at 30 feet during ascent to the surface. |
| Adapted from the US Navy Diving Manual. |
Table VII. US Navy Treatment Table 6A - Initial Air and Oxygen Treatment of Arterial Gas Embolism¶*
Depth
(feet) | Time
(minutes) | Breathing
Media¥ | Elapsed
Time
(hrs:min) |
|---|
| 165‡ | 30# | air | 0:30 |
| 165 to 60 | 3ft/min | air | 0:34 |
| 60 | 20 | O2§ | 0:54 |
| 60 | 5 | air | 0:59 |
| 60 | 20 | O2 | 1:19 |
| 60 | 5 | air | 1:29 |
| 60 | 20 | O2 | 1:44 |
| 60 | 5 | air | 1:49 |
| 30 | 15 | air | 3:49 |
| 30 | 60 | O2 | 4:49 |
| 60 to 30 | 30 | O2 | 2:19 |
| 30 | 15 | air | 2:34 |
| 30 | 60 | O2 | 3:34 |
| 30 to 0 | 30 | O2 | 5:19 |
| * | Treatment of arterial gas embolism where complete relief obtained within 30 min at 165 feet. Use also when unable to determine whether symptoms are caused by gas embolism or severe decompression sickness. |
| † | Descent rate--as fast as possible. Ascent rate--1 ft/min. Do not compensate for slower ascent rates. Compensate for faster ascent rates by halting the ascent. |
| ‡ | Time at 165 feet-- includes time from the surface. |
| § | If oxygen breathing must be interrupted as a result of adverse reaction, allow 15 minutes after the reaction has subsided and resume schedule at the point of interruption. |
| ¥ | Caregiver breathes oxygen during ascent from 30 feet to the surface unless he has had hyperbaric exposure within the past 12 hours, in which case he breathes oxygen at 30 feet. |
| ¶ | Extensions: Table 6A can be lengthened up to 2 additional 25 minute periods at 60 feet (20 minutes on oxygen and 5 minutes on air) or up to 2 additional 75 minute oxygen breathing periods at 30 feet (15 minutes on air and 60 minutes on oxygen), or both. If Table 6A is extended either at 60 or 30 feet, the tender breathes oxygen during the last half at 30 feet and during ascent to the surface. |
| # | If complete relief is not obtained within 30 min at 165 feet, switch to Table 4, consulting with a Diving Medical Officer if possible. |
| Adapted from the US Navy Diving Manual. |
Table VIII. US Navy Treatment Table 4 - Air or Air and Oxygen Treatment of Type II Decompression Sickness or Arterial Gas Embolism*¥¶
Depth
(feet) | Time | Breathing
Media§ | Total
Elapsed
Time (hrs:min) |
|---|
| 165† | _ to 2 hr# | Air | 2:00‡ |
| 140 | _ hr | Air | 2:31 |
| 120 | _ hr | Air | 3:02 |
| 100 | _ hr | Air | 3:33 |
| 80 | _ hr | Air | 4:04 |
| 60 | 6 hr | Air or Oxygen/Air | 10:05 |
| 50 | 6 hr | " | 16:06 |
| 40 | 6 hr | " | 22:07 |
| 30 | 12 hr | " | 34:08 |
| 20 | 2 hr | " | 36:09 |
| 10 | 2 hr | " | 38:10 |
| 0 | 1 min | " | 38:11 |
| * | Treatment of worsening symptoms during the first 20 minute oxygen breathing period at 60 feet on Table 6, or when symptoms are not relieved within 30 minutes at 165 feet using treatment Table 3 or 6A. |
| † | Descent rate--as rapidly as possible. Ascent rate--1 minute between stops. |
| ‡ | Time 165 feet--includes time from the surface. |
| § | If only air available--decompress on air. If oxygen available, patient begins oxygen breathing upon arrival at 60 feet with appropriate air breaks. Both tender and patient breathe oxygen beginning 2 hours before leaving 30 feet. |
| ¥ | Ensure life support considerations can be met before committing to a Table 4. Internal chamber temperature should be below 85 degrees F 29.4° C. |
| ¶ | If oxygen breathing is interrupted, no compensatory lengthening of the table is required. |
| # | If switching from treatment table VIA at 165 feet, stay the full 2 hours at 165 feet before decompressing. |
| Adapted from the US Navy Diving Manual. |
Table IX. US Navy Treatment Table 7- Oxygen/Air Treatment of Unresolved or Worsening Symptoms of DCS or AGE *†‡¶@
| Depth (feet) | Time (hours) | Breathing Media¥ | Total
Time (hours) |
|---|
| 60 | 12 hr minimum¥ -no maximum | Oxygen 20 min, air 5 min | 12 hours |
| Ascend 3 ft/hr or two ft every 40 min | 6 hours | | 18 hours |
| Ascend 2 ft/hr# | 10 hours | | 28 hours |
| Ascend 1ft/hr | 16 hours | | 44 hours |
| 4 feet | 4 hour stop | | 48 hours |
| Ascend 1 ft/hr | 4 min | | 48 hours/4 min |
| * | Used for treatment of unresolved life threatening symptoms after ini valign=toptial treatment on Table 6, 6A, or 4. |
| † | Use only under the direction of a Diving Medical Officer. |
| ‡ | Table begins on arrival at 60 feet. Arrival at 60 feet is accomplished by initial treatment on Table 6, 6A or 4. If initial treatment has progressed to a depth shallower than 60 feet, compress to 60 feet at 25 ft/min to begin table 7. |
| § | Maximum duration at 60 feet is unlimited. Remain at 60 feet a minimum of 12 hours unless overriding circumstances dictate earlier decompression. |
| ¥ | Patient begins oxygen breathing periods at 60 feet. Caregiver need breathe only chamber air throughout. If oxygen breathing is interrupted, no lengthening of the table is required. |
| ¶ | Minimum chamber O2 concentration: 19%. Maximum chamber CO2 concentration: 1.5% SEV (12 mm). Maximum temperature: 29.4°C. |
| # | Decompression starts with a 2 foot upward excursion from 60 to 58 feet. Decompress with stops every 2 feet for the times shown on the above profile. Ascent time between stops is approximately 30 seconds. Stop time begins with ascent from deeper to next shallower step. Stop at 4 feet for 4 hours and then ascend to the surface at 1 ft/minute. |
| @ | Ensure chamber life support requirements can be met before committing to this table. |
| Adapted from the US Navy Diving Manual. |
Table X. US Navy Treatment Table 5 - Oxygen Treatment of Type I DCS*¥
Depth
(feet) | Time
(minutes) | Breathing
Media¶ | Total
Elapsed
Time (hrs:min) |
|---|
| 60† | 20 | O2§ | 0:20‡ |
| 60 | 5 | Air | 0:25 |
| 60 | 20 | O2 | 0:45 |
| 60to30 | 30 | O2 | 1:15 |
| 30 | 5 | Air | 1:20 |
| 30 | 20 | O2 | 1:40 |
| 30 | 5 | Air | 1:45 |
| 30 to 0 | 30 | O2 | 2:15 |
| * | Treatment of Type I decompression sickness when symptoms are relieved within 10 minutes at 60 feet and a complete neurological exam is normal. |
| † | Descent rate--25 ft/min. Ascent rate--1 ft/min. Do not compensate for faster rates by halting the descent. |
| ‡ | Time at 60 feet begins on arrival at 60 feet. |
| § | If oxygen breathing must be interrupted, allow 15 minutes after the reaction has entirely subsided and resume schedule at point of interruption. |
| ¥ | If oxygen breathing must be interrupted at 60 feet, switch to Table 6 upon arrival at the 30 foot stop. |
| ¶ | Caregiver breathes air throughout unless he has had a hyperbaric exposure within the past 12 hours, in which case he breathes oxygen at 30 feet. |
Table XI. US Navy Treatment Table 3 - Air Treatment of Type II DCS or Arterial Gas Embolism*
Depth
(feet) | Time
(minutes) | Breathing
Media | Total
Elapsed
Time
(hrs:min) |
|---|
| 165† | 30 min | Air | 0:30‡ |
| 140 | 12 min | Air | 0:43 |
| 120 | 12 min | Air | 0:56 |
| 100 | 12 min | Air | 1:09 |
| 80 | 12 min | Air | 1:22 |
| 60 | 30 min | Air | 1:53 |
| 50 | 30 min | Air | 2:24 |
| 40 | 30 min | Air | 2:55 |
| 30 | 720 min | Air | 14:56 |
| 20 | 120 min | Air | 16:57 |
| 10 | 120 min | Air | 18:58 |
| 0 | 1 min | Air | 18:59 |
| * | Treatment of Type II symptoms or arterial gas embolism when oxygen unavailable and symptoms are relieved within 30 minutes at 165 feet. |
| † | Descent rate--as rapidly as possible. Ascent rate--1 minute between stops. |
| ‡ | Time at 165 feet--includes time from the surface. |
| Adapted from the US Navy Diving Manual. |
References
- Polak B, Adams H: Traumatic air embolism in submarine escape training. U.S. Naval Med. Bull. 30: 165-177, 1932.
- Francis TJR, Smith D (eds): Describing Decompression Illness. Bethesda, Undersea and Hyperbaric Medical Society, 1987.
- Boyle R: New pneumatic experiments about respiration. Phil. Trans. R. Soc. London 5: 2011-2031, 1670.
- Vann RD, Thalmann ED: Decompression physiology and practice, in Bennett PB, Elliott DH (eds): The Physiology and Medicine of Diving. London, WB Saunders, 1993, ed 4, pp 376-432.
- Elliott DH, Moon RE: Manifestations of the decompression disorders, in Bennett PB, Elliott DH (eds): The Physiology and Medicine of Diving. London, WB Saunders, 1993, ed 4, pp 481-505.
- Flynn ET: Decompression sickness, in Camporesi EM, Barker A (eds): Hyperbaric Oxygen Therapy: A Critical Review. Bethesda. Undersea and Hyperbaric Med. Soc. , 1991, pp 55-74.
- Francis TJR, Gorman DF: Pathogenesis of the decompression disorders, in Bennett PB, Elliott DH (eds): The Physiology and Medicine of Diving. London, WB Saunders, 1993, ed 4, pp 454-480.
- US Navy Diving Manual. Commander Naval Sea Systems Command Publication 0994-LP-001-9010. Washington DC, US Government Press, 1993, Revision 3, Vol 1, Chapter 8.
- Thalmann ED, Buckingham IP, Spaur WH: Testing of Decompression Algorithms for Use in the US Navy Underwater Decompression Computer (Phase I). US Navy Experimental Diving Unit Report 11-80, 1980.
- Thalmann, ED: Phase II Testing of Decompression Algorithms for Use in the US Navy Underwater Decompression Computer, US Navy Experimental Diving Unit Report 1-84, 1984.
- Thalmann ED: Development of a Decompression Algorithm for Constant 0.7 ATA Oxygen Partial Pressure in Helium Diving. US Navy Experimental Diving Unit Report 1-85, 1985.
- Thalmann ED: Air-N2O2 Decompression Algorithm Development. US Navy Experimental Diving Unit Report 8-85, 1986.
- Kizer KW: Delayed treatment of dysbarism: A retrospective review of 50 cases. JAMA 247: 2555-2558, 1982.
- Yap CL: Delayed decompression sickness--the Singapore experience, in Proc Joint S Pacific Underwater Med Soc and Republic Singapore Navy Underwater Med Conf. SPUMS J Suppl, 1981.
- Kindwall EP: Decompression sickness. In: Davis JC, Hunt TK (eds): Hyperbaric Oxygen Therapy. Bethesda, Undersea Medical Society, 1977, pp 125-140.
- Butler FK, Pinto C: Progressive Ulnar Palsy as a late complication of decompression sickness. Annals Emerg Med 15: 738-741, 1986.
- Air decompression, in Department of the Navy: US Navy Diving Manual, NAVSHIPS 0994-001-9010, Vol 1. Air Diving. Washington, DC: Department of the Navy, 1991 pp 7-1 to 7-24.
- Behnke, AR: Analysis of Accidents occurring in training with the submarine "lung". U.S. Naval Medical Bull. 30: 177-184, 1932.
- Schaefer KE, Nulty WP, Carey C, et al: Mechanisms in development of interstitial emphysema and air embolism on decompression from depth. J. Appl. Physiol. 13: 15-29, 1958.
- Malhotra MC, Wright CAM: Arterial air embolism during decompression and its prevention. Proc. R. Soc. Med. B154: 418-427, 1960.
- Mader JT, Hulet WH: Delayed hyperbaric treatment of cerebral air embolism. Arch. Neurol. 36: 504-505, 1979.
- Catron PW, Dutka AJ, Biondi DM, et al: Cerebral air embolism treated by pressure and hyperbaricoxygen. Neurology. 41: 314-315, 1991
Suggested Readings
Arthur DC, Margulies RA: A short course in diving medicine. Annals Emerg Med 16: 689-701, 1987.Ball R. Effect of severity, time to recompression with oxygen, and retreatment on outcome in forty-nine cases of spinal cord decompression sickness. Undersea and Hyperbaric Medicine 20:133-145, 1993.
Berghage TE, Durman D: US Navy Air Decompression Schedule Risk Analysis. Bethesda, MD: Naval Medical Research Institute Technical Report, NMRI #80-1, 1980.
Boettger ML. Scuba diving emergencies: Pulmonary overpressure accidents and decompression sickness. Annals Emerg Med 12: 563-567, 1983.
Boussuges A, Thiriion P, Molenat F, et al: Neurologic decompression illness: A gravity score. Undersea and Hyperbaric Medicine 23:151-155, 1996.
Boycott AE, Damant GCC, Haldane JS: The prevention of compressed-air illness. J Hyg Camb 8: 342-443, 1908.
Bove AA, Moon RE, Neuman TS: Nomenclature of pressure disorders. Classification of the decompression disorders: time to accept reality. DCI/DCS: Does it matter whether the Emperor wears clothes? Undersea and Hyperbaric Medicine 24:1-4, 1996. Editorials.
Bove AA: The basis for drug therapy in decompression sickness. Undersea Biomed Res 9: 91-111, 1982.
Bracken MB, et al: A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal injury. New Eng J Med 322: 1405-1412, 1990.
Catron PW, Flynn ET Jr: Adjuvant drug therapy for decompression sickness: A review. Undersea Biomed Res 9: 161-74, 1982.
Cross SJ, Thomson LF, Jennings KP, et al: Right-to-left shunt and neurological decompression sickness in divers.
Lancet ii 568, 1989. Letter.
Cross SJ, Lee HS, Thomson LFet al: Patent foramen ovale and subaqua diving . BMJ 304: 1312, 1992. Letter.
Davis JC, Kizer KW: Diving medicine, in: Auerbach PS, Geehr EC (eds): Management of Wilderness and Environmental Emergencies, 2nd edition. St. Louis, The C.V. Mosby Co., 1989.
Dewey AW, Jr: Decompression sickness, an emerging recreational hazard. N Engl J Med 267: 759-65; 812-20, 1962.
Dick APK, Massey EW: Neurologic presentation of decompression sickness and air embolism in sport divers. Neurology 35: 667-671. 1985
Edmonds C. Barotrauma, in Strauss R.(ed): Diving Medicine. New York, Grune & Stratton, 1976.
Gorman DF: Decompression sickness and arterial gas embolism in sports scuba divers. Sports Medicine 8: 32-42, 1989.
Green RD, Leitch DR: Twenty years of treating decompression sickness. Aviat Space Environ Med 58: 362-6, 1987.
Hall ED: Lazaroids: Mechanisms of action and implication for disorders of the CNS. Neuroscientist, 3:42-51, 1997.
Johnston RP, Broome JR, Hunt PD, et al: Patent foramen ovale and decompression illness in divers. The Lancet 348: 1515, 1996. Letter.
Kelleher PC, Pethybridge RJ, Francis TJR: Outcome of neurological decompression illness: development of a manifestation based model. Aviat, Space, and Environ Med 67: 654-658, 1996.
Kindwall EP: Diving emergencies, in Kravis TC (ed): Emergency Medicine Aspen Systems Corporation, Rockville, Maryland, 1983.
Kizer KW: Dysbaric cerebral air embolism in Hawaii. Ann Emerg Med 16: 535-41, 1987.
Knauth M, Ries S, Pohlmann S, et al: Cohort Study of multiple brain lesions in sport divers: Role of a patent foramen ovale. BMJ 314: 701-705, 1997.
Krzyzak J: A case of delayed-onset pulmonary barotrauma in a scuba diver. Undersea Biomed Res 14: 553-61, 1987.
Mebane GY, Dick AP: DAN Underwater Diving Accident Manual. Divers Alert Network, Duke University, 1985.
Mitchell SJ: The role of lignocaine in the treatment of decompression illness: A review of the literature. SPUMS Journal 25:182-194, 1995.
Moon RE, Sheffield PJ: Guidelines for Treatment of Decompression Illness. Aviat Space Environ Med 68:234-43, 1997.
Moon RE, Camporesi EM, Kisslo JA: Patent foramen ovale and decompression sickness in divers. Lancet
1: 513-514, 1989.
Moon RE, Sheffield PJ, (eds.): Treatment of Decompression Illness. 45th Workshop of the Undersea and Hyperbaric Medical Society, June 1996.
Neblett LM: Otolaryngology and sport scuba diving. Update and guidelines. Annals Otology, Rhin and Laryng. Supplement 115: 1-12, (a great article) 1985.
Rivera JC. Decompression sickness among divers: An analysis of 935 cases. Military Medicine, pp 314-334, April 1964.
Roydhouse N: 1001 disorders of the ear, nose and sinuses in scuba divers. Can J Appl Spt Sci 10: 99-103. 1985.
Schaefer KE, McNulty WP Jr., Carey C, Liebow AA. Mechanisms in development of interstitial emphysema and air embolism on decompression from depth. J Appl Physiol 13: 15-29, 1958.
Strauss RH. Diving Medicine: State of the Art. Amer Rev Resp Dis 119: 1001-1023, 1979.
Thalmann ED in Moon RE, Sheffield PJ eds. Treatment of Decompression Illness. 45th Workshop of the Undersea and Hyperbaric Medical Society, June 1996; pp 75-95.
Weeth JB. Management of underwater accidents. JAMA 192: 215-219, 1965.
Wilmshurst P, Byrne JC, Webb-Peploe MM. Relation between interatrial shunts and decompression sickness in divers.
Lancet II: 1302-1306, 1989.
Weathersby PK, Homer LD, Flynn ET: On the likelihood of decompression sickness. J Appl Physiol 57: 815-25, 1984.
Weathersby PK, Survanshi SSM, Homer LD, Parker E, Thalmann ED: Predicting the time of occurrence of decompression sickness. J Appl Physiol 72:1541-1548, 1992.
Weathersby PK, Survanshi SS, Hays JR, et al: Statistically based decompression tables III. Comparative Risk Using US Navy, British, and Canadian Standard Air Schedules. Bethesda, MD: Naval Medical Research Institute Technical Report, NMRI #86-50, 1986.
Wilmshurst: Patent foramen ovale and subaqua diving . BMJ 1312, 1992. Letter.
Wilmshurst P: Transcatheter occlusion of foramen ovale with a button device after neurological decompression illness in professional divers. The Lancet 348: 752-753, 1996.
Wilmshurst P: Brain damage in divers (editorial). BMJ 314: 689-690, 1997.
sumber ;
Ernest S. Campbell, MD, FACS, Orange Beach, Ala scuba-doc.com
Ditayangkan ulang oleh dr. Erick Supondha /Hyperbaric & Diving medicine Consultant.
Hiperbarik, hyperbaric jakarta, ahli hiperbarik jakarta, hyperbaric doctor jakarta indonesia
021 99070050